Childbirth Journey
Last month of pregnancy
Continuing from where this post left off, we started week 36 with a mini scare. This day coincided with my last day of work, in which I had a routine OB appointment. The nurse took my blood pressure and saw a reading above 140/90, which put me in the risk zone for pre-eclampsia. Afraid I’d have to rush over to the delivery room right away, Simon and I panicked. Thankfully the doctor ordered a non-stress test, some labs, and a 24-hour urine sample, all of which came out fine. Whew, we still had a bit more time before the baby came.
However, because my protein levels were elevated, I had to return to the clinic to retake these tests at least once a week until the due date. My OB also recommended an induction at 39 weeks to prevent the rising blood pressure and protein levels from progressing into an actual pre-eclampsia diagnosis. Fully prepared to get pregnancy over with, I was glad to have a deadline in mind.
At home, I wrapped up work and started my maternity leave. I took things slow and observed changes in my body everyday: small headaches come and go, blood pressure rises and lowers, energy levels ebb and flow. The baby put pressure on my uterus area and I spent a lot of evenings unable to get out of bed. Pelvic mobility stretches help though. At night, I did perineal massages to prep for birth. I also spent a lot of time reading about other people’s induction experiences on Reddit, which unfortunately just triggered more anxiety and fear about childbirth pains.
On the day before my scheduled induction, I woke up and took a blood pressure reading… 148/91. Panic set in. I called Labor and Delivery in shock, who tells me to go to the nearby clinic to get this number verified in case my cuff isn’t calibrated. I quickly took my last pregnancy photo and scurried over to the clinic. It turned out my cuff was indeed reading higher, and they sent me back home. Relieved, Simon started playing piano while I read a book. Our minds were on what we’d be having for lunch when suddenly I got a call from a doctor at the hospital, telling me to come for induction as soon as possible. My diastolic pressure from the clinic reading was nevertheless in the 90s, which meant:
I was officially diagnosed for pre-eclampsia. We had to get this baby delivered.
Induction
12:00 Pm
After that phone call, we eat a quick lunch, grab our remaining things, and drive over to the hospital. I’m calm and optimistic because we already had our panic moment weeks ago. We arrive at the hospital and get admitted.
1:00 PM
We start continuous fetal monitoring, draw blood for labs, put in the IV, and check on the cervix. At this point I was dilated to 2 cm.
2:30 pm
Induction starts with a balloon catheter that will be checked at the 6 and 12 hour mark. I turn down painkillers despite what the internet warned. (Balloon insertion did not hurt.) I also start taking misoprostol pills, my first of 6 pills to be administered every 2 hours.
4:00 PM
We put on a movie to watch and I start to feel some cramps, which the nurse tells me are small contractions. The sensation felt like the need to poop, along with soreness in my back that would come and go, but nothing unmanageable. I happily bounce on my yoga ball, energetic, excited, and confident about every little win in natural pain management.
7:30 pm
I discover a small amount of bloody show, which indicates that the cervix is opening.
9:30 PM
We attempt to sleep as nurses come in every once in a while to continue giving me misoprostol pills and adjust the finicky fetal monitor bands around my belly that slip off every move I make.
Midnight
Baby is officially 39 weeks of gestational age.
4:15 am
The balloon foley is taken out at the 12-hour mark, and my cervix dilated to 5 cm, although labor hadn’t quite started. The midwife breaks my bag of waters to speed things up.
Labor
4:45 am
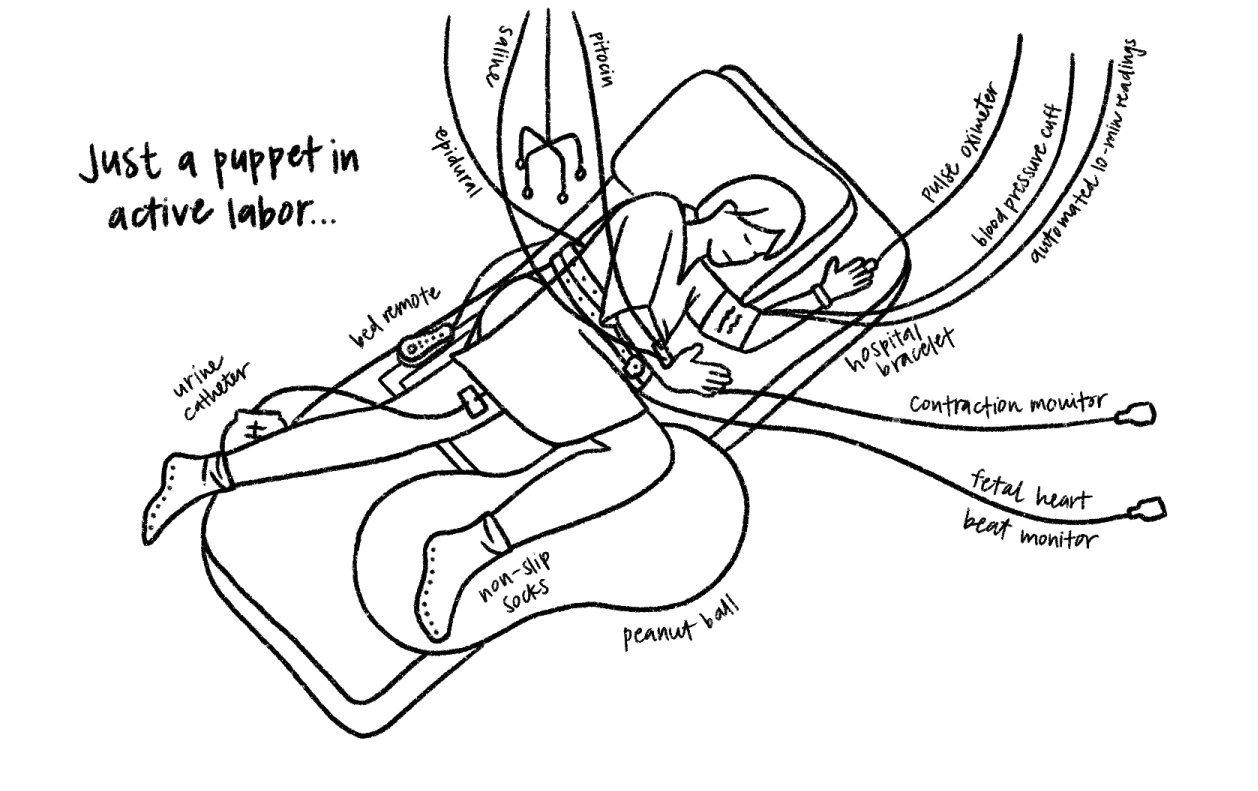
Contractions intensify so I ask a nurse for a TENS unit, which slightly numbs the pain. I get tired of being confined to the hospital bed, so I switch to a portable fetal monitor as I move around the room and stretch into every position to open up my hips. Each contraction, I double over onto my hands and knees and take 4 long breaths to withstand the pain. I ask Simon apply counter-pressure onto my lower back during each peak, a coping mechanism that proved more effective than anything else.
10:00 AM
I’m dilated to 6 cm, which officially starts active labor. Going from 5 to 6 cm didn’t seem like much progress, but the midwife tells me my hard work in the first stages of labor paid off because my natural body had finally caught up to my artificially induced dilation.
I was tired but since my preference was to deliver unmedicated, I wanted to see how much further along I could progress before taking Pitocin.
10:45 AM
A whole night of labor had me physically fatigued in a way I’ve never felt before, and I had no remaining energy to keep going for an indeterminate amount of time. I ask for an epidural and Pitocin. The anesthesiologist stuck the needle into my back and the switch was like night and day as I finally relaxed for the first time in hours. Why didn’t I do this earlier?, I kept thinking to myself.
2:30 PM
I was finally 10 cm dilated. It was time to start pushing. 😨
Delivery
2:50 pm
I start pushing, or rather, learning how to push. When she detected a contraction coming on via the monitor, the nurse would tell me to take a short breath in and exhale 3 times in quick succession as I pushed. The sensation was the same as pushing out a big poop. Soon I started feeling a constipated feeling coming on every few minutes and realized those were the waves of contractions. The nurse holds my legs with every push, yelling at me to push harder, while Simon feeds me water and juice in between peaks. It takes me a while to learn to push from the right place in my body as I switch between laying and squat positions. An hour in, I start to doubt my ability to actually do this. Every round of pushing felt like two steps forward, one step back. At this point I’m physically exhausted and losing faith. Can’t you just vacuum her out of me? I ask the nurse. She says there is no need, I was getting close.
I knew giving birth would be hard, but pushing was definitely the hardest part. The nurse was screaming in my face every push, counting down the ten seconds in which I was supposed to push with max capacity. This energy-intensive technique certainly did not help me relax nor push properly. The breathing pattern also felt unintuitive, because during pregnancy I’ve had to learn to NOT push bowel movements and here we were doing the exact opposite. Similarly, the fast-paced shallow exhale was the opposite of the deep yoga breath I know and love. At some point I chucked up some juice because I pushed so hard it came out the wrong end.
4:00 pm
Aided by a mirror, I make progress (we could see the top of baby’s hairy head through a lime-sized opening!) and the on-call OB comes to apply mineral oil and prepare for the actual delivery. Towards the end, a team of 5 different people come in SWAT team-style to get various stations ready. After a few more rounds of pushing, I open my eyes to see Simon tearing up. She must be almost here, I realize. I close my eyes and go into my last contraction and push. Even though I can’t see anything, I hear the excitement in the voices of everyone around me.
5:21 pm
Our baby girl is born! I hear a cry and feel a huge sense of relief. They plop her onto my chest and I’m in shock. I couldn’t believe this living being had actually been inside me the whole time. I always thought I’d cry in this moment, but instead I stare at her in awe, marveling at every feature. I brush her tiny purple fingers and examine her vernix-stained head of hair. I watch intently as she stops crying to open one eye to gaze up at us for the first time.
As I get distracted by the miracle we created, the doctor quickly delivers my placenta, cuts the umbilical cord, and stitches up my first-degree perineum tear. Thankfully I felt none of this happening due to the surge of hormones and emotions running through me. We start “golden hour” skin-to-skin time with the baby.
7:00 pm
The nurse teaches me how to breastfeed (by slapping her mouth onto my boob the second she opens it) and baby girl has her first “meal,” a few drops of colostrum. Half an hour later, we move to the recovery room where we stay for two more nights until discharge.
All the tubes I collected during active labor, post-epidural. I’ve never felt so fragile and stiff.
I went into childbirth with a ton of anxiety. To me, giving birth was the climax of the journey, something I’d been anticipating for a long time with varying degrees of fear. I’m one who likes having control of my body — I treat it well and it typically treats me well in return. But when it started doing unexplainable things (e.g. developing high blood pressure, fatiguing after a few hours), I panicked. And that panic never truly settled because of the uncertainty of the induction. How successful was it? When can I expect to actually go into labor?
As I prepped my birth plan, I also felt the pressure to challenge myself and do something hard — deliver this baby unmedicated. However, when the moment came, it was important to ultimately listen to my body. I couldn’t muster the physical strength to keep pushing through a seemingly never-ending stretch of prolonged labor. I couldn’t let my ego get in the way of hurting my body or the baby.
Through the hormones and roller coaster of oxytocin, I am surprised my brain still worked 100%. I could understand what the nurses were talking about, ask informed questions, and remind them of things they themselves forgot to do. I am glad to have done my research and know exactly what was coming every step of the way.
All in all, however difficult or unexpected, giving birth is an experience to be lived. Shoutout to Kaiser Redwood City for taking such good care of us during our 3-day stay. 10/10 would choose this hospital next time around. (Fingers crossed I forget the the pain of childbirth so there can be a next time around.)
Our hospital bag must-haves
Bag to take home all the free hospital stuff
Lotion/mosturizer for yourself
Toothbrushes, paste, floss
Your own food and snacks (more than you think you need) because hospital food is not good
A pillow you like (I brought my thick foam pillow)
Breastfeeding pillow
Nursing bra or tank
Some type of nursing cups to protect from nipple pain or trauma
Baby nail clippers or file
Soft toilet paper that you like
Peri bottle
Extra-long phone charger
Slippers
Baby going home outfit (that allows them to buckle into carseat)
Cameras
What I would’ve done differently
Shower before I left for the hospital, and make sure my hair is clean
Bring more snacks
Ask nurses to turn down the volume of continuous fetal monitor
Tell nurses that my skin is sensitive to adhesive tape (used for saline lock, epidural, catheters). Those rashes took days to heal after I got home, and hurt more than my perineum.
Rest when I get the chance to, and save my energy for the hard part
Practice different breathing techniques for pushing ahead of time
Take more stuff from hospital. Ask for more of the things you need to use for recovery at home (maxi pads, disposable underwear, ice packs, sitz bath, incontinence bed pads, swaddles, diapers, wipes, nasal bulb, nipple cream)
Make Simon swear on his life to take candid photos/videos without being prompted
“Birth is the ultimate act of love, strength, and creation.”














Trusting my body, becoming a mother, and rebuilding myself during a long, transformative year.